All prescription medications discussed in here were prescribed by my PCP to me for the purposes described.
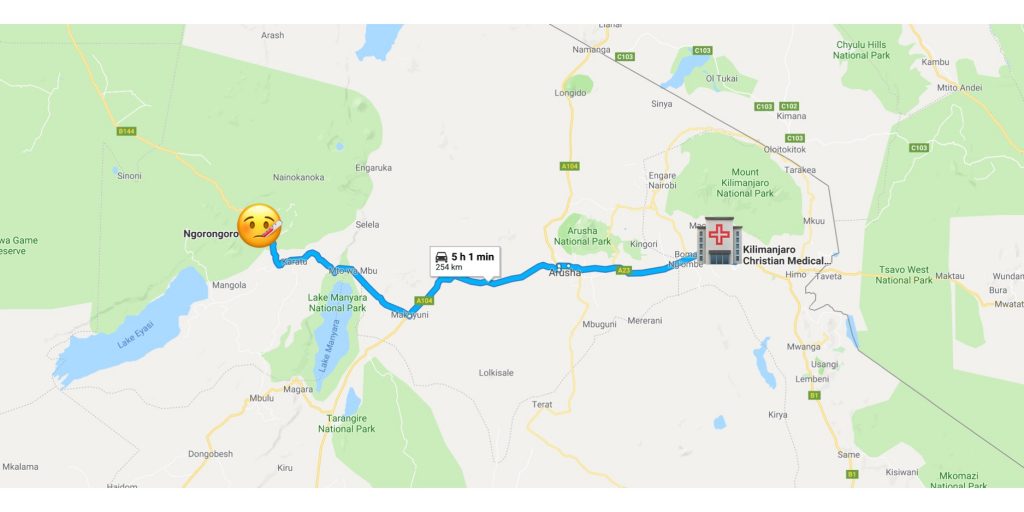
Here’s a quick write up about some of my risk assessment and mitigation efforts for an upcoming trip to Moshi, Tanzania. I’m there to complete a professional development program with a clinical rotation at Kilimanjaro Christian Medical Centre. I will be there approximately 7 weeks with 5-6 days per week spent on shift in the hospital. While I had originally hoped to spend longer in Tanzania to explore, it didn’t work with my schedule for December. The upside of spending the majority of my time in the hospital means I don’t have the risks associated with other activities I might have done, such as climbing Kilimanjaro or Kitesurfing in Zanzibar.

My general approach with risk identification is to talk with those that have experience in the area, check a few organization websites (listed below), do some broad google searches (“security XXXXX” “safety XXXXX” “attack XXXXX” “crime XXXXX”) then follow any leads I find there, and check travel forums like Trip Advisor and Flyertalk. Based on the trip I may check specific organizations working in the area and see if they have recommendations for their personnel. It’s worth remembering that most countries do not have homogenous risks across the nation so figuring out what is specific to the area, for me Moshi, is part of the equation. Moshi has lower crime rates than Dar Es Salaam and Arusha.
International Association for Medical Assistance to Travelers
CDC Travelers’ Health Clinician Resources
US Department of State Overseas Security Advisory Council reports
WHO Outbreak Bulletins
DoD Vaccine Recommendations by AOR
I’m not going to get in to basic travel safety stuff here. Much of the broad information readily available is decent and covers making yourself a less obvious target and traveling smart.
For my trip the risks that I believe to be most likely or have the greatest consequence are:
Mosquito Borne Illness
Occupationally contracted virus
Major trauma (crime or motor vehicle accident)
Food and Waterborne Diseases
Gastrointestinal Illness / Traveler’s Diarrhea
Comms issue complicating one of the above
References
Mosquito Borne Illness

General Precautions
I am bringing a permethrin treated mosquito bed net which can be hung above my bed and tucked under the mattress. When I am sleeping I will be in a very lightweight cotton sleeping bag liner. I have DEET 30% skin safe bug repellent and lightweight long sleeved shirts and pants.
Malaria
Here’s a great fact sheet from the WHO with specifics about malaria in mainland Tanzania. 100% of the cases of malaria are P. Falciparum (Pf). 1
It’s important to know which species of Plasmodium is active in the area as some have developed resistance to particular medications and some species has more complicated treatments. Pf and Plasmodium knowlesi (Pk) are the worst of the Plasmodium family as they can cause rapidly progressive illness and death. P. vivax and P. ovale require treatment to address the hypnozoite forms which cause relapsing infection by remaining dormant in the liver. 2
My chemoprophylaxis will be Atovaquone-proguanil Hcl 250-100mg which is the generic of Malarone. I am starting it 2 days before the trip, will take it daily during the trip, and daily for 7 days once I leave the area.
Dengue
General precautions as there is no chemoprophylaxis available. There is one Dengue vaccine on the market (Dengvaxia) but it is not FDA approved. The WHO put out a great position paper in September 2018 that details the studies of the vaccine and the problems with it. Biggest issue identified so far is that for individuals who have not been exposed to dengue before receiving the vaccine actually have a higher risk of developing severe dengue after the vaccine should they become naturally infected with dengue. 3 In my case, I would be one of those people not previously exposed but likely to have a bad time if I got the vaccine. For those who have already been exposed the vaccine seems to be reasonably safe and shows a decrease in hospital admissions for dengue.
Chikungunya
General precautions as there is no chemoprophylaxis or vaccine available.
Occupationally contracted virus
I will utilize best practices regarding hand washing, use of PPE, handling of sharps, and disposal of waste products. Beyond that here are some disease specific thoughts.
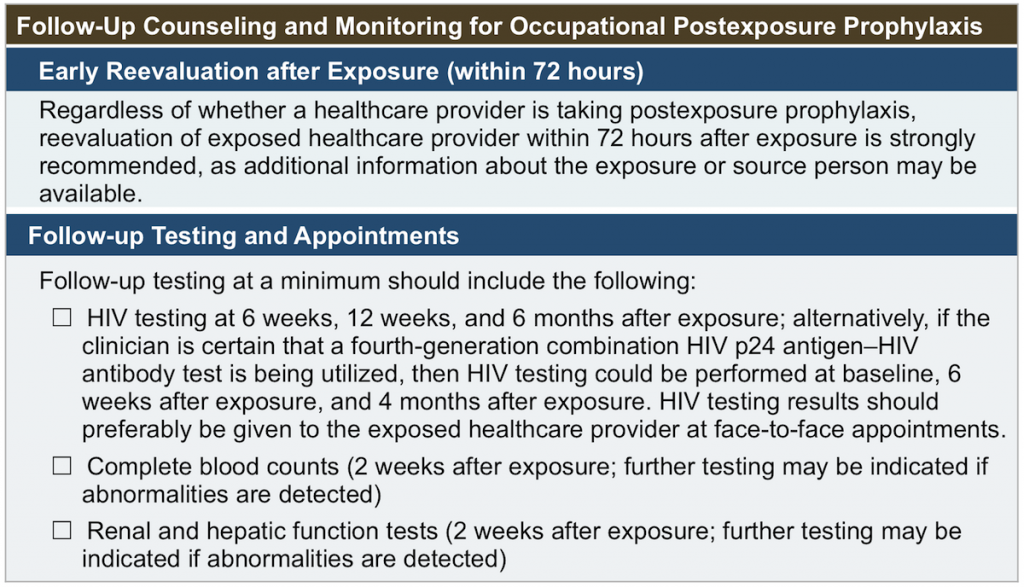
HIV
2.1% of the population in Moshi has HIV. 4 As a point of comparison 0.3% of the US population had HIV in 2015. 5 Exposure to HIV is a concern and to reduce the impact should I be exposed I am bringing Occupational Post Exposure Prophylaxis (oPEP) based on the guidelines from University of California San Francisco Clinician Consultation Center. 6 My oPEP will be 28 day course of Truvada ([co-formulated Tenofovir DF (Viread®; TDF) 300mg + emtricitabine (Emtriva™; FTC) 200mg]) and Tivicay (dolutegravir 50mg). PEP is generally considered to be 99% effective when taken as soon as possible after exposure. 7 Some of the available research that evaluated the effectiveness of PEP found that those who seroconverted while on PEP were men engaging in unprotected receptive anal intercourse. I’m looking for specific data but I suspect those individuals have a greater overall risk of seroconversion from exposure than one does in a healthcare setting. With unprotected receptive anal sex there can be microtears increasing ease of contraction plus exposure of the mucus membrane to the HIV virus in the semen. Compare that exposure to a health care provider being splashed with blood on an abrasion or experiencing a needle stick. A study out of South Korea found that over a 5 year period where there were 1,076 in-hospital occupational blood exposures there was only one Hepatitis C Virus infection and no Hepatitis B or HIV infections. 8
My worst case scenarios would be receiving a HIV+ blood transfusion or injuring myself during point of injury treatment for a significant trauma. I’ll still take the oPEP, get tested after, consult with my PCP, and see how things turn out. It’s worth noting, I know my HIV status (negative) going in to the trip. If you are sexually active it’s worth having regular STI testing including HIV.
Hepatitis B Virus (HBV)
I’ve previous received the HBV vaccine and will utilize best practices.
Hepatitis C Virus (HCV)
No vaccine available, I will utilize best practices.
Tuberculosis (TB)
TB is highly endemic in Tanzania although many patients have latent TB. Granted, people who have active TB sometimes go to hospitals and I’ll be working in a hospital… Recognition of a patient that potentially has TB and use of appropriate PPE for myself and them will be key here. There is a TB vaccine but it is not commonly given in the US. 9 I might consider the vaccine for another trip or if I knew I was going to be specifically working with more patients that have active TB. If I was going to be working in a more limited clinic I’d likely bring a few N95 masks just in case sourcing them locally was difficult or impossible.
Major trauma (crime or motor vehicle accident)
Moshi is a bit safer than other parts of Tanzania however as a whole Tanzania is a reasonably safe and stable country. There have certainly been robberies targeting visitors and crimes committed against LGBT individuals.
My transportation to and from the airport is provided by a trusted driver with an established history. I won’t be renting a vehicle or motorbike while there. I am also not engaging in any wilderness or adventure activities.
As far as treatment goes, I always carry a small trauma kit (SWAT TQ, QC Combat Gauze, Compressed Gauze, Gloves, Light, Rescue Hook, Tape) plus have packed a SOFTT-W. I am packing another trauma kit more focused on moderate injuries which will have some elastic bandages, gauze, and tape. I will be staying a few blocks from the major hospital in the area which is also where I will be working.
For pain management I am bringing APAP and Ibuprofen to address mild-moderate pain and Mobic for something more severe.
Food and Waterborne Diseases
Drink bottled water, eat fully cooked meat and produce, avoid suspect eateries, evaluate food prep and storage areas when possible, wash hands when possible or use alcohol hand sanitizer, peel produce that can be peeled, avoid raw fruits and vegetables.
Typhoid Fever
I got the Typhim Vi vaccine in 2017 and it’s good for 3 years. 10
Paratyphoid Fever
No vaccine available.
Hepatitis A
I got the Vaqta vaccine in 2017 and it’s good for 25 years. 11
Hepatitis E
No vaccine available.
Cholera
There is an active outbreak with 80 cases and 2 deaths ~250km west of Moshi in Ngorongoro District. 12 A live attenuated oral vaccine is FDA approved. I looked in to before my Iraq trip in 2017 and might obtain it the next time I’m going to an area with Cholera. Frankly, I forgot to follow up about getting it do for this trip. The vaccine does present some challenges at it is a live virus and gets handled a bit differently in the pharmacy and the recipient sheds live cholera through the GI tract for a bit after receiving the vaccine.
Gastrointestinal Illness & Traveler’s Diarrhea
Prevention will be through precautions regarding food and water and taking bismuth subsaliciylate 2 tabs (262 mg/tab) QID. 13 Bismuth subsaliciylate is somewhere between 50-60% effective in preventing Traveler’s Diarrhea. I’m pretty happy with that. Sure 100% would be better but even a small reduction of my risk with no real downside is good to me. Treatment will focus on oral rehydration with salt and glucose supplementation as needed from Nuun tablets + sugar 14 first then the WHO homemade ORS solution. 15 To make rehydration more efficient I will have Loperamide 1mg tablets to decrease GI motility and Ondansetron 4mg ODT to reduce vomiting.
Should the diarrhea persist beyond 2-3 days or I develop bloody stool I will suspect a bacterial infection rather than viral and utilize the course of Levofloxacin 750mg I was prescribed. The most common cause of dysentery is shigellosis 16 and the most common cause of Traveler’s diarrhea is E. coli. 17 Levofloxacin is effective against shigellosis and E. coli.
Comms issue complicating one of the above
Following the PACE methodology here’s my comms plan
Primary: iPhone 7 on the T-mobile ONE plan
In Tanzania, the plan affords me free texting and data plus voice calls at $0.25 per minute. Per T-mobile customer service they guarantee 2G in Moshi, possibly 3G. With my T-mobile SIM card I will be connecting to Airtel or Halotel networks. There are a few restaurants and cafes in Moshi which provide wifi as well. With texting and data I will be able to use standard SMS as well as What’s App and Signal.
Alternative: iPhone
Try different messaging apps and swap SIM card for a second locally purchased card or use the phone on wifi only if cell isn’t work.
Contingency: Nokia 105 Unlocked Feature Phone
The Nokia 105 is a simple phone that makes voice calls and sends texts (very inefficiently). I will purchase a SIM card on the ground and preferably grab one from a different network than my iPhone will be connecting to.
Emergency: Delorme InReach SE
The InReach allows for messaging with location attached through the Iridium satellite network which has global coverage. The messages can be sent from the device alone or through an app when paired with the iPhone. Additionally the device has an SOS feature.
I have multiple digital and physical copies of the emergency numbers I need including the embassy, evacuation insurance, and in case of emergency contact.
References
- World Health Organization Country Profile, Malaria, United Republic of Tanzania (Mainland) Link
- Centers for Disease Control and Prevention Malaria Clinical Guidance Link
- World Health Organization Dengvaxia Summary of Research and Vaccine Position Paper, pg 474 for WHO position Link
- All Africa News Link
- CDC Basic Statistics Link
- University of California San Francisco Clinician Consultation Center Link
- CATIE Link
- Occupational blood exposures in health care workers: incidence, characteristics, and transmission of bloodborne pathogens in South Korea BMC Public Health Link
- CDC Tuberculosis Link
- Consumer Information Leaflet PDF Link
- electronic Medicines Compendium Link
- WHO Weekly Bulletin on Outbreaks and Other Emergencies PDF Link
- Prevention and Self-Treatment of Traveler’s Diarrhea Clinical Microbiology Reviews Link
- Nuun Nutritional Information Link
- WHO homemade ORS Link
- Family Practice Notebook Link
- Family Practice Notebook Link