If this is your hypothermia management plan for a trauma patient they will become intimately familiar with the lethal triad (hypothermia, acidosis, and coagulopathy) and potentially death from a preventable cause, hypothermia.
A small space blanket can have a role in hypothermia treatment or prevention but as a stand alone item is insufficient.
For a patient with severe accidental hypothermia (eg cold water immersion) or severe trauma they are simply not generating enough heat and the thin, disposable space blanket does a minimal job of trapping that heat. Further heat is still being lost to the environment through conduction (direct contact with a colder surface), convection (cold air movement through gaps in the space blanket), and to a certain degree radiation (space blanket does not trap 100% of heat generated by the body).
Before we go further we should consider that this patient may not walk out so making them easier to carry will help us out. Lay out your movement device on the ground and proceed from there. The movement device could be an improvised soft litter, commercial soft litter, tubular webbing litter, commercial device like a SKEDCO or Foxtrot, or any number of other solutions, just put handles on your patient.
When constructing a hypowrap we must think about the ways the body is losing heat and specifically counter those ways while adding more heat to the system.
Let’s start by creating as close to a closed system as possible to prevent further heat loss.
When cool air passes over the skin heat is lost via conduction so one of our countermeasures needs to interrupt this. A sturdy tarp creates a great foundation to build the hypo wrap on as the tarp is a moisture and wind barrier. 10’x12′ is a decent size as it allows you to wrap the patient up without having too much extra bulk. The hypo wrap will be assembled diagonally on this so one corner of the tarp corresponds to the patient’s head and the opposite corner corresponds to their feet.
Heat is conducted away from the body by direct contact with a surface colder than the body such as the earth, metal or plastic stretcher, or the floor of a vehicle. We need to separate the patient from this with padding. A sleeping pad designed for this purpose in camping works well but blankets, sleeping bags, pine boughs, or extra clothes can work as well. If you have determined that a long spine board is essential for your patient, please read most of the research surrounding this as it likely is more harmful than beneficial, do an excellent job padding the board so it does not serve as a giant heatsink for your patient.

The next layer can be the patient placed inside a sleeping bag and then in to a heavy duty survival blanket such as a Blizzard Blanket or SOL Bivvy. Any of the reflective mylar products that are, when new, are closer in size to a 1L water bottle will out perform the deck of playing card sized blankets. The sleeping bag and survival blanket trap heat and radiate it back to the patient.
Prior to insertion in to the sleeping bag consider how you will continue to monitor the patient. If they are uninjured and experiencing accidental hypothermia perhaps mental status will be adequate but for our trauma patients we want to be able to trend vitals.
A pulse oximeter can be placed on the patient’s finger and the arm bent so their palm is wresting on the opposite shoulder. Pro tip, using a loop of paracord loosely secure the pulse ox to the patient’s wrist so that when it falls off you only have to find their wrist to find the pulse ox not dig through the hypowrap. If the patient’s fingers are cold initially do not expect an accurate reading if you get one at all. This should change as their condition improves.
On the opposite arm a BP cuff with removable gauge and stethoscope can be placed allowing for repeat BP checks. A quality digital wrist BP cuff might be considered here as suggested in the Prolonged Field Care Working Group Nursing Care Clinical Practice Guidelines.
Placing a fleece cap on the patient’s head also helps limit heat lost through the very vascular scalp.
At this stage the patient can be placed on the padding in their survival blanket and sleeping bag and wrapped up with the tarp. The sides of the tarp are folded towards the patient and the foot flap is folded up to cover the sides. If the patient will be moved secure with the tarp with duct tape, paracord, or a rope litter.
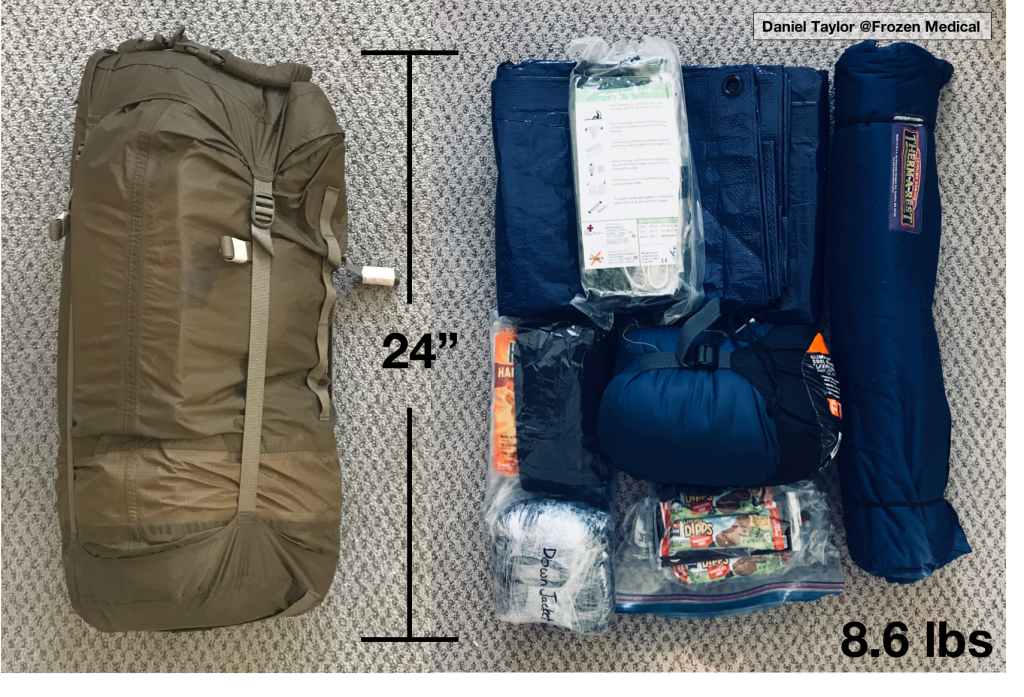
Here’s what I would consider to be the most minimal hypowrap kit I could responsibly carry in a professional capacity.
10 x 12’ tarp
Blizzard Survival Blanket
Hand and body warmers with fleece cap in ziplock
~30F sleeping bag,
Down jacket
Granola bars and chocolate bars (readily available glucose)
Therm-a-rest pad
All contained in an Outdoor Research compression dry bag
Weight: 8.6lbs (3.9kg)
The above kit was able to be secured below a medic pack with two quick release buckles.
The more extreme the trauma is likely to be or if I am expecting winter conditions without access to a vehicle then I would upgrade the sleeping bag and add a source of heat safe for use close to the body (Ready Heat Blanket).
A note on the hot packs, these are included as a comfort item and not designed for active rewarming. If applied directly to skin with decreased perfusion due to cold injury or physiologic shock these hot packs can cause thermal injury unperceived by the patient due to blunted pain receptors.
In the event of accidental hypothermia the patient is still capable of generating heat, but their metabolic rate of heat production was less than the rate that heat was being taken away by the environment. Supporting the patient’s own heat generation through providing simple sugars may speed their recovery hence the inclusion of granola bars and chocolate.
Commercial hypothermia management kits are a great option as well although personally I like being able to customize exactly what I am carrying.
Examples such as the Hypothermia Prevention and Management Kit and Hypothermia Management Kit have proven themselves with the US military and should be considered depending on your budget and space constraints. Knowing how to construct a quality hypowrap using only locally sourced materials is critical though.
A SKEDCO Sked litter is an awesome tool to have access to. It’s bulky, weighs 20+ lbs depending on setup, and expensive ($600+ USD new), but if you find yourself moving a patient over anything more than a hundred feet you will be extremely happy to have it. It can be a drag, carry, or lower/hoist device.
You can lay the Sked down as your first layer and place the tarp on top then follow on as you would normally. When stored the Sked rolls up and fits in the backpack shown above. The contents of a decent hypo wrap will fit in the center void of the rolled Sked. I found that I couldn’t stuff the sleeping bag down while in it’s compression sack so I took the sleeping back out, placed loosely in several heavy duty contractor bags and turned the whole thing in to a sad lumpy tamale shape which then did fit down the center of the Sked. That setup worked in British Columbia doing snowmobile based medical response.
If you are able to carry a second set of diagnostic equipment I’d consider adding that to the center of the Sked as well so that when your patient is wrapped up with a BP cuff, stethoscope, and pulse oximeter you have used the one from the Sked not your primary diagnostics kit.
This final suggestion might seem dark, but it’s practical and multipurpose. A quality body bag with handles can take the place of the tarp and potentially the litter.
The bag shown here retails for $95 which seems steep but I can assure you that using improvised body bags is terrible and if your patient hasn’t expired the bag will do an outstanding job as part of your hypowrap. Follow the same steps just substitute the body bag for the tarp.
When working as a remote site medic I do consider remains recovery, when safe and practical, to be part of my mandate. If attempting to repatriate the remains will foreseeably cause additional risk or injuries I cannot do so. Recovering the remains feels like one of the last ways I can honor the patient I was unable to help and potentially support their family. There’s also the potential for something to be learned from the patients death through autopsy and study of their personal effects (dive computer, GPS watch, cell phone).