Felt an explosion for the first time. Shook the house a little.
Glossary:
ISOF: Iraqi Special Operations Forces
TSP: Trauma Stabilization Point
MSF: Doctors without Borders
VBIED: Vehicle Borne IED
Daesh: Arabic name for IS/ISIS/ISIL, possibly derogatory, largely interchangeable with IS/ISIS/ISIL. There’s more to it than that, but can we just generally agree, fuck those guys?
IDP: Internally Displaced People. The term for Iraqis forced from there homes but still within the borders of Iraq. Often referred to as “refugees” but they don’t meet the legal definition of that term.
WHO: World Health Organization
Felt an explosion for the first time. Shook the house a little.
I get that this seems very cavalier and may come across as false bravado, but those words are what I wrote later that day. My bar to be worried about something needed to be fairly high otherwise I wouldn’t have been functional. I used the reactions of those around me to help calibrate my sense of threat. Many of the folks I was serving along side, Westerners and Iraqis, had been in war zones for months if not years. Some of them were absolutely numb to aspects of the world around them but they also hadn’t gotten themselves killed yet. If no one seemed worried I tried to follow suit. I have no doubt that if one of the airstrikes had landed outside our door I would have been a bit less cool. Hopefully still functional, but certainly a little more… animated. I never had to face my own mortality as a reality which might dramatically change how I feel about the whole experience.
Like most emergency medicine providers James developed the skill of being able to sleep whenever time permitted. I believe he had been in country for a little over two months at this point and most of that time was spent in active conflict areas. He’d earned a nap. When we got word that patients would be arriving someone would nudge him and he would be right back up ready to help out.
Busy day.
Teen with infected head wound maggots and severe facial swelling.
I may talk more about this child’s condition in a specific case study, but I’ll allow an image to do most of the speaking for the time being. This picture was taken with patient permission by Claire Thomas, one of the photojournalists who embedded with us. She and the other photojournalists I interacted with deserve their own post. Almost all of them were incredible. They documented many horrors that would otherwise go unnoticed and are able to speak for those who cannot speak for themselves.

The child suffered a deep scalp laceration which became severely infected and the infection traveled down the right side of his face leading to so much swelling the eye lid was closed over the eye. His eye sight was grossly intact which was promising. Although the presentation is alarming if the infection was aggressively treated there was a good chance he could heal without lasting effects. We prioritized him to go to a hospital with services for pediatrics rather than an IDP camp. Our biggest concern was the infection spreading to the eye or the brain.
During a lull in the activity Kyirsty and I were able to visit a WHO mobile clinic that had setup across the street from us. The mobile clinic was able to provide primary care and address some minor issues. Having them working with us was a huge help. We referred patients to them and they sent patients to us. The staff are all Iraqi and incredibly friendly.

I give the mobile clinic staff a lot of credit given their proximity to the fighting. Based on my memory and Live Map archives I believe we were 1-1.5km from the fighting that day. The clinic staff are “regular” healthcare providers. These are not thrill seeking, risk taking, emergency medicine types like myself and my compatriots in the TSP. I would honestly be surprised if they had learned how to use a tourniquet or had access to one. Despite that they were close enough that they could have been targeted by a suicide bomber or been unlucky enough to have been hit by a wildly off course airstrike. We didn’t discuss these risks but there is no way they weren’t aware of them. I am very appreciative of them and the WHO for making that mobile clinic possible.
Child with open femur fx, teen with ex fix [external fixation] at left humerus
Receiving a patient with an external fixation of a fracture was very surprising. Placing an ex fix is a surgical procedure usually done by an orthopedic surgeon. This is one of several times we received patients that had been treated by some of the hospitals or clinics Daesh stood up. Rumor was that they had contracted some foreign doctors, there’s no question some of their recruits had medical training, and under threat of death they forced many Iraqis with medical training to care for their patients. This last scenario happened to one of the doctors I worked along side.
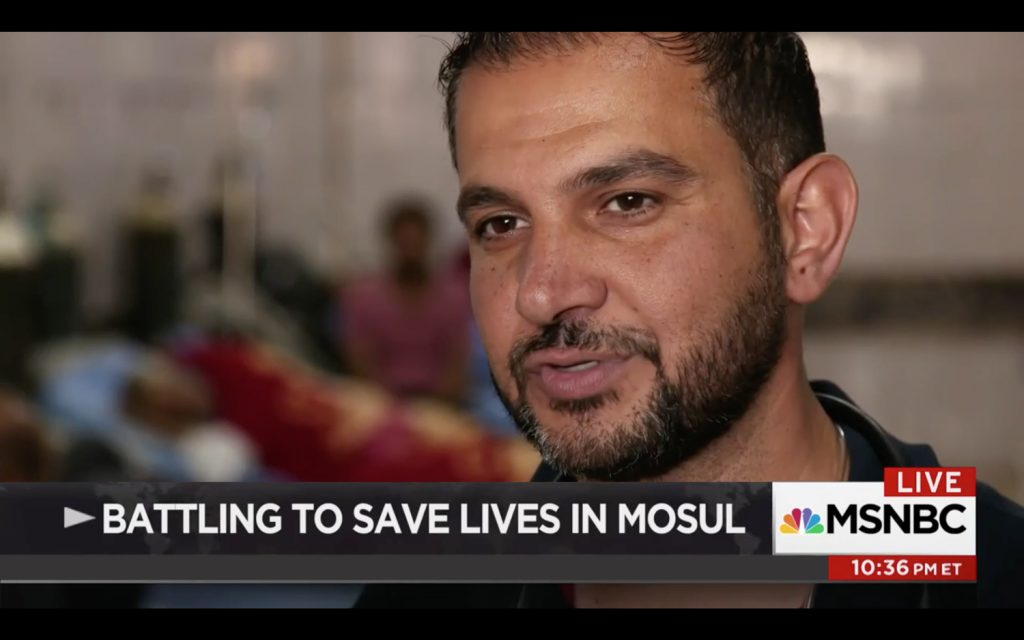
The folks featured at the beginning of the video are ones I worked with in Mosul. You can skip to 2:46 to see Dr. Alkassab, but I think the entire video, just under 6 minutes long is worth watching.
Iraqi Army Intelligence mentioned that they held the belief that given the severely limited supplies available at this point (Daesh was fully surrounded and had been so for several weeks) those receiving advanced care, eg chest tubes or external fixation, were likely Daesh fighters or close family of high ranking Daesh soldiers. In the case of the child, I don’t know one way or the other. Some of those that came in with advanced care were confirmed to have a connection to Daesh.
ISOF [soldier] with a chest wound and GSW to thigh with arterial bleeding – Kyirsty starting a line during transport – bad ass – I bagged [breathed for them with a bag valve mask] the patient.
Starting an IV during transport is usually a little challenging given patient positioning in the ambulance and the added movement from typical traffic and road conditions. Magnify all of those factors a few times and you are getting closer to the conditions we experience when Kyirsty started the IV. I think the one we had coming out the TSP may have gotten dislodged and we didn’t have an IO to place in the rig.
open head injury with brain matter [visible] he started with good breathing and purposeful movement and equal pupils, we delivered him [to the hospital] with purposeful movement
Visible brain matter is one of those findings we often equate with injuries incompatible with life. The fact that this guy took a rifle round to the skull and was still talking when he made it to the TSP speaks to how close we were and how good the Iraqis were at rapidly evacuating patients. If I had the same patient on a civilian ambulance I wouldn’t be surprised if enough time elapsed between the shooting and my arrival on scene (delayed by safety focused protocols and communication issues) that the patient would have expired or at a minimum be unresponsive.
he [the previously described patient] became combative in the TSP so I sedated him with Ketamine after arguing with the Iraqi medics since they don’t like to give ketamine especially for head injuries
There used to be concerns about giving Ketamine to patients with head injuries due to increased Intracranial Pressure (ICP). This has been largely debunked but I wouldn’t be surprised to meet the same resistance in an ambulance in the US.
Trench entrapment: is ketamine safe to use for sedation in head injury?
Ketamine for rapid sequence induction in patients with head injury in the emergency department.
I weighed the loss of an accurate mental status assessment against the harm he could do to himself by remaining combative. I was concerned his thrashing around would lead to increased ICP and could become indistinguishable from hypoxia. Sedating him and not going on the ambulance with him could lead to hypoxia due to positional issues so I was committing myself to go with him. Sending patients without a provider was common practice given the shear number of patients we saw relative to the number of providers we had combined with the distance (20-60 minutes) of hospitals from our location. Feeling that we had adequate people to allow me to maintain his airway during transport I made the call to push the Ketamine. He calmed down significantly, experienced no apnea, and remained hemodynamically stable during the transport. He was able to withdraw from noxious stimuli. If memory serves he may have had snoring respirations once or twice during the trip to the hospital but those were quickly corrected with a modified jaw thrust and NPA.
Different place to sleep tonight, at the mosque which is a [previous] TSP, good food, chatting with Kyirsty and James
Where I stayed that night, and the rest of my time in Mosul, was a mosque that housed the other half of the GRM team. When the fighting was closer to the mosque it had been a TSP and still served as the primary one overnight. There were fewer ISOF soldiers at this location, but we still had ample security. The layout of the compound allowed us to spread out a little more.
The main worship space made for a great clinic to receive traumas and do sick call for the neighborhood. Two smaller buildings outside the worship space, but inside the compound walls provided additional sleeping quarters. There were several places to bathe and a nice gas powered cooking surface. Plus the roof of the mosque made for a nice place for the team to gather and unwind at the end of the day. We would sit there and watch the explosions for a few hours.
Iraqi ground operations largely stopped overnight due to limited night vision, but airstrikes continued and occasionally Daesh would launch a counter attack under cover of night.






Ran one MCI (danger close airstrike) in shorts, flip flops and a tshirt then went back to the roof only to do another one (vbied) which we had seen detonate. 12-14 patients between the two events.
We had maybe a minute or two heads up before the patients arrived so we scrambled off the roof, I grabbed my TSP “battle belt”, and went in to the Mosque to start seeing patients. Three of us plus a few ambulance drivers to help herd people was enough to manage both incidents. I wish I had a picture of myself during those MCIs. I’m guessing my neon white legs would have made the picture impossible to obtain though.

